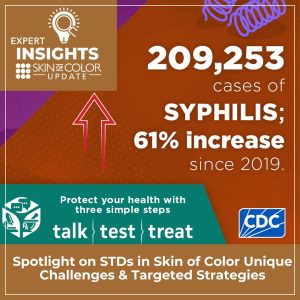
At the 2024 Skin of Color Update, Theodore Rosen, MD, FAAD, highlighted the critical role dermatologists play in recognizing and treating sexually transmitted diseases (STDs), many of which present with skin findings. His talk focused on the disproportionate burden of STDs in patients with skin of color, the unique clinical presentations of STDs, and the importance of early detection and equitable access to care.
- Epidemiology & Disparities: In the U.S., 2.5 million STDs are diagnosed annually. African American, Hispanic, American Indian, and Alaska Native populations experience disproportionately high rates of STDs likely due to barriers in healthcare access and lack of knowledge of STD care.
- Syphilis: Cases of primary, secondary, and congenital syphilis continue to rise, with a record number of congenital cases in 2022. Secondary syphilis in patients with skin of color may mimic psoriasis or appear as nodular or annular lesions. Early recognition is essential to reduce congenital syphilis.
- Monkeypox (Mpox): Rates have declined since 2022, but Black and Hispanic men who have sex with men remain disproportionately affected. Full vaccination is underutilized due to lack of availability, and resistance to tecovirimat is emerging.
- HSV (Herpes Simplex Virus): Overall rates are declining, but non-Hispanic Black individuals remain disproportionately affected. Hypertrophic/vegetative HSV-2, more common in immunocompromised patients with skin of color, requires biopsy, appropriate immunostaining, or viral culture (PCR) to make a diagnosis. Treatment requires multimodal therapy.
- Other STDs: Chancroid, donovanosis, and lymphogranuloma venereum are now rare in the U.S., and mostly limited to specific populations.
- Testing & Resources: Patients can access free or at-home STD testing through CDC resources.
Key Takeaway: Rising STD rates, especially syphilis, highlight the urgent need for targeted screening, culturally competent care, and better education and prevention strategies for patients with skin of color.
This session summary was written by Dr. Olive Osuoji and published on Next Steps in Derm.
Register for Skin of Color Update for more medical dermatology updates.