Andrew F. Alexis, MD, MPH
Eliot F. Battle, MD
Next Steps in Derm recently published a highlight from the Skin of Color Update Virtual 2020 poster session.
Thin on Top: A Cross-Sectional Analysis of the Top Black Hair Loss Videos and Black Hair Loss Treatment Videos on YouTube
Esther B. Henebeng BS¹, Uzoamaka Okoro MD, MSc², Ogechi Ezemma BA¹, Kristina Monteiro PhD¹, Afiya M. Mbilishaka PhD³, Chesahna Kindred MD, MBA4
¹The Warren Alpert Medical School, Brown University, Providence, RI, ²Dwight D. Eisenhower Army Medical Center, Fort Gordon, GA, ³University of the District of Columbia, Washington, DC,4Howard University College of Medicine, Washington, DC
Alopecia, or hair loss, is a prevalent concern for both men and women, that has substantial impact on quality of life.¹ Many forms of alopecia in Black women are associated with or worsened by traumatic styling practices such as braiding, weaving, thermal or chemical hair straightening. Therapy is tailored to the specific diagnosis and can include altering haircare practices, topical or oral medications (ex. minoxidil), and in-office treatments (ex. intralesional injections, hair transplant).² However, studies have shown a considerable amount of Black women are concerned physicians may not understand their hair and fail to engage in discussions about hair issues for this reason.³ More than 50% of Black women experience hair loss, with a majority of women searching for treatment options from online resources instead of seeking care from a primary care physician or dermatologist.4 YouTube is one of the most frequently used websites, with 77% of Black adults using the social media platform.5 Although dermatologists have established an online presence, approximately 75% of the top dermatology-related videos on YouTube are from non-dermatologist sources.6 This is particularly concerning because videos from third parties have been found to suffer from incomplete information, overall poor quality, and can contribute to potential harm or delay in appropriate diagnosis.6,7
Behbahani et al showed that YouTube is a highly utilized resource for hair loss treatment information, but found no significant difference between the overall quality of board certified dermatologist and non-physician videos.7 However, videos from lay media or individuals have been shown to have lower accuracy in comparison to videos from health care sources.8 Examination of top YouTube videos regarding “hair” and “hair loss” demonstrated very few videos displaying more textured or tightly coiled hair types associated with Black hair. Consequently, our project will evaluate the accuracy, quality, viewer engagement, and viewer experience of “Black hair loss” and “Black hair loss treatment” videos on YouTube.
YouTube was searched for the following: “Black hair loss” and “Black hair loss treatment” on June 18, 2020. The first 60 videos per search term were examined and categorized into health care or non-health care sources. Two independent raters evaluated each video with four validated instruments: 1) Accuracy in Digital Health, 2) Accuracy Scale, 3) Armstrong Viewer Assessment, and 4) Global Quality Scale.8 Viewer engagement ratio was defined as (number of likes + dislikes + comments) / total views. Discrepancies between coders were resolved through discussion. Duplicate and non-English videos were excluded. Significant differences between health care and non-health care sources were determined using Mann- Whitney U test.
Our search yielded a total of seventy-eight unique YouTube videos. Three videos made no claims to assess accuracy and were excluded from analysis (*).
Twenty-two (28.2%) of the videos were from health care sources and fifty-six (71.8%) from non-health care sources. Health care sources were made up of dermatologists, nondermatologist medical doctors, and university/professional organizations. Non-health care sources included individuals, hairstylists, companies, and lay media. Speakers in 45 of the YouTube videos (57.7%) self-identified as Black based on video content or a publicly accessible social media post. Of the 45, there were only 2 videos categorized as health-care sources that had a self-identified Black speaker.
There are over 20 million total views for the top 78 videos on Black hair loss and Black hair loss treatment. These videos typically range from 1 minute to 10 minutes long, with varying levels of engagement. Videos by Black speakers were found to have higher levels of engagement (0.02 ± 0.02, P = <0.001). Many of the videos by non-health care sources were inaccurate or made claims with no evidence supported by PubMed literature review. A few speakers encouraged viewers to try potentially harmful practices to stimulate hair growth (ex. Vicks VapoRub to scalp, prolonged protective styles, intermittent fasting or detoxing). When compared to non-health care sources, health care sources had lower mean numbers of views (81,965 vs 330,113, P = 0.008). Furthermore, health care sources were less engaging than non-health care sources (0.01±0.01 vs 0.02 ±0.02, P = 0.012), but more accurate (Accuracy in Digital Health: 3.77 ±0.43 vs 2.00 ±1.57, P = <0.001; Accuracy Scale: 3.91 ±0.30 vs 2.15 ±1.25, P = <0.001). Most inaccuracies from health care sources were primarily associated with the promotion of a product or treatment that does not have proven efficacy. Fewer inaccuracies were related to incorrect comments regarding hair physiology and causes of hair loss. Nevertheless, health care sources provided a superior viewer experience (Armstrong Viewer Assessment: 3.09 ±0.53 vs 2.55 ±1.01, P = 0.023) and were of higher quality (Global Quality Scale: 3.64 ±0.85 vs 2.47 ±1.09, P = <0.001) in comparison to non-health care sources.
Source: JDD Online
The Journal of Drugs in Dermatology recently featured the article, The Relevance of Vitamin D Supplementation for People of Color in the Era of COVID-19, authored by Skin of Color Virtual Update faculty, Pearl E. Grimes MD, and Andrew F. Alexis MD MPH along with Nada Elbuluk MD MSU.
Introduction
African Americans (AA) and other people of color are dying at highly disproportionate rates from COVID-19. The statistics are staggering: in New York City alone, per 100,000 population, death rates in AA were 92.3, and in Hispanics 74.3, compared to 45.2 in Whites and 34.5 in Asians.1 Similar numbers have been reported in other cities and are presumed underestimations, given limited racial/ethnic reporting. In the states currently releasing the number of COVID-19 deaths by race and ethnicity, Blacks make up roughly 13 percent of the population, but 27 percent of the deaths. According to the American Public Media Research Lab, the rate of COVID-19 deaths nationally for Blacks has been reported as twice the rate of deaths of Asians and Latinos in the US and more than 2.5 times the rate for White residents.
Socio-economic reasons, pre-existing comorbidities, work circumstances, inconsistent healthcare access, stress, and decreased immunity, amongst other factors, have been posited as reasons for this shocking disparity. People of color, in particular AA and Hispanics, are more likely to be uninsured and to be frontline workers during the COVID-19 pandemic. This is compounded by the fact that comorbidities such as hypertension, diabetes, asthma, obesity, and cardiovascular disease are more common in AA and are also associated with higher COVID-19 mortality rates. Emerging evidence suggests that Vitamin D deficiency may represent another risk factor for poor outcomes from COVID-19.
Relevance of Vitamin D
Vitamin D is a secosteroid hormone synthesized in the skin following exposure to UVB ultraviolet radiation where it mediates the conversion of 7-dehydrocholesterol to pre-Vitamin D3. Following transport to the liver, it is hydroxylated to 25(OH)D, the primary circulating form typically used to measure serum Vitamin D levels. 25(OH)D is subsequently converted to the biologically active form 1,25, dihydroxy vitamin D in the kidneys by 1-alpha hydrolase. This active form binds to its nuclear Vitamin D receptor to induce the transcription of over 200 genes, affecting a wide range of physiologic functions.
Multiple studies have documented significant Vitamin D deficiency in people of color, especially in AA. Heavily melanized skin retards the synthesis of Vitamin D and necessitates longer periods of sun exposure for adequate synthesis of Vitamin D. Ginde et al. assessed demographic differences and trends of Vitamin D insufficiency in a US population.2Serum 25(OH)D levels were compared over two time periods (1988–1994 and 2001–2004) from the Third National Health and Nutrition Examination Survey (NHANES III) data base including two large populations (n=18,883 and n=13,369, respectively). Non-Hispanic Blacks had a significantly higher prevalence of Vitamin D deficiency, increasing in severity in the later data base. Recent NHANES data from 2011–2014 further documented the high risk of deficiency in non-Hispanic Blacks. In a recent prospective cohort study of 14,319 subjects, an estimated 65.4% of non-Hispanic Blacks were deficient in Vitamin D, compared to 29% of Hispanics and 14% of non-Hispanic Whites.3
Vitamin D deficiency has been shown to be a risk factor for many of the comorbidities that disproportionately plague AA including diabetes, hypertension, cardiovascular disease, autoimmune diseases such as lupus erythematosus, as well as aggressive forms of breast and prostate cancer.4 While the classic role of Vitamin D involves calcium and phosphorus homeostasis for healthy bone metabolism, it exerts a spectrum of pleotropic effects impacting cell growth, differentiation, inflammation, and immune regulation. Healthy levels of Vitamin D have been linked to significantly reduced mortality and improved health outcomes. Numerous investigations document the prolific role of Vitamin D in antimicrobial defense and modulation of the innate and adaptive immune responses. It mediates the induction of key antimicrobial peptides in the respiratory epithelium including cathelicidin (LL37) and beta defensins, which destroy invading organisms. In addition, Vitamin D inhibits the production of pro-inflammatory cytokines including IL-2, IFN-γ, TNF-α, and IL-6, while promoting Th2 responses by increasing IL-4, IL-5, and IL-10 production, hence skewing T cell responses to a down regulated, anti-inflammatory state.4
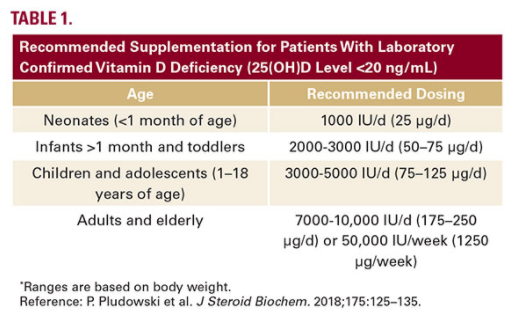
For the general population, the US Institutes of Medicine (IOM) recommends Vitamin D supplementation at doses that vary according to age and are based primarily on bone health. Current IOM supplementation recommendations are 400 IU (10ug) for infants, 600 IU/d (15ug) for children, adolescents, and adults, and 800 IU/d (20ug) for adults aged over 70 years to maintain a 25(OH)D concentration of 20ng/mL or higher. However, in individuals who are deficient in Vitamin D (25(OH)D level <20 ng/ mL), of which patients with skin of color are at a higher risk, supplementation is considerably higher. These recommendations are summarized summarized in Table 1.5
Conclusions
Source: Next Steps in Derm
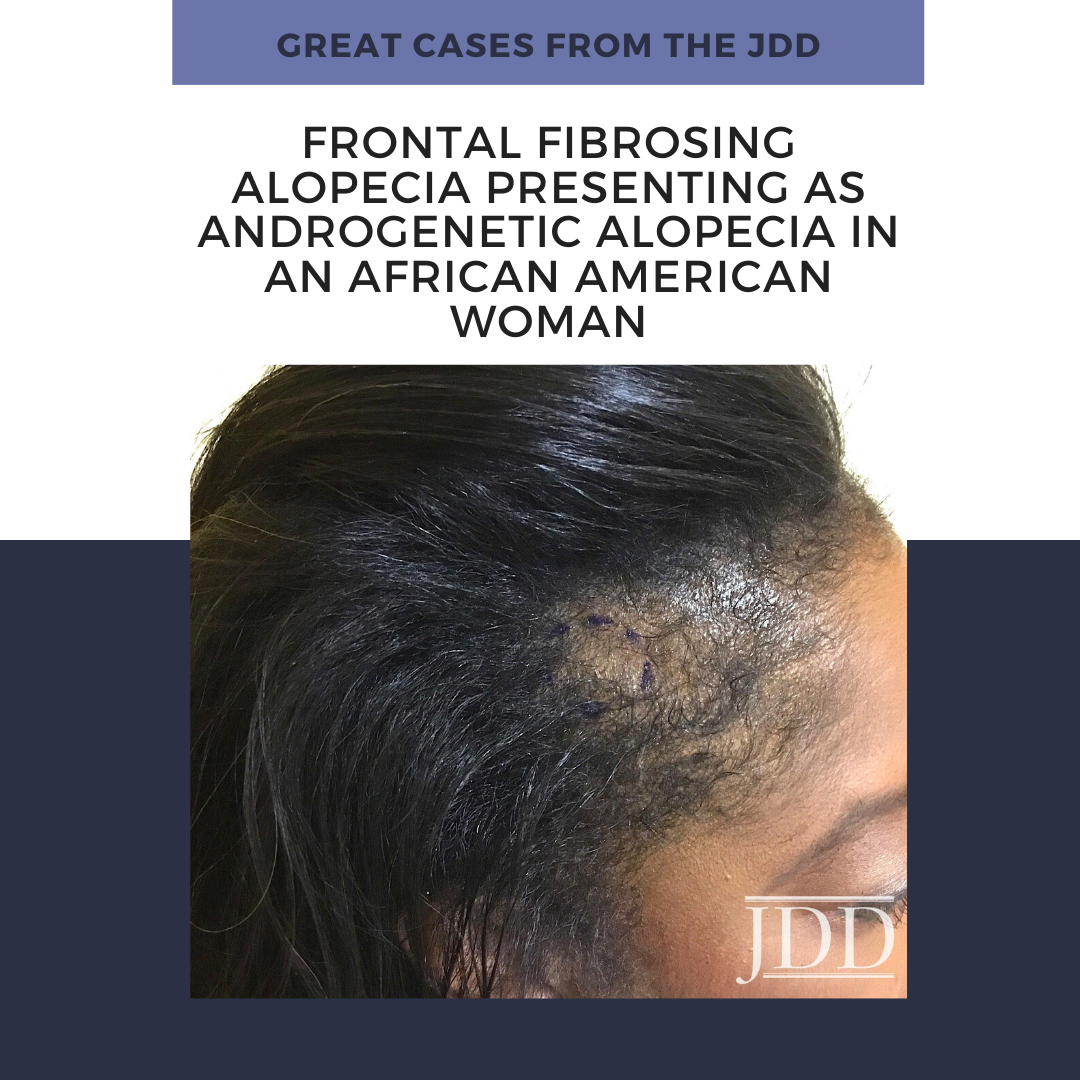
Frontal fibrosing alopecia (FFA) is a primary lymphocytic cicatricial alopecia that is currently regarded as a variant of lichen planopilaris. FFA has historically been considered rare in black patients, in whom traction alopecia, central centrifugal cicatricial alopecia, and androgenetic alopecia are frequently assumed to be more common. JDD author Kimberly Huerth, MD, ME describes a case of FFA in a black woman that both clinically resembled androgenetic alopecia and lacked many of the physical exam and dermoscopic findings associated with FFA. In doing so, she highlights the need for physicians to have a high index of suspicion for FFA in any black patient who presents with frontotemporal alopecia.
A 53-year-old African American woman presented with a 6-month history of asymptomatic, moderately severe hair loss along the frontal hairline, which had not stabilized or improved with minoxidil 2% solution BID. Physical exam revealed decreased hair density affecting the frontal scalp, suggestive of androgenetic alopecia (Figure1). Dermoscopic examination showed decreased follicular ostia without perifollicular scaling or erythema. Eyebrow alopecia, facial papules, and glabellar red dots were absent, and there was no associated loss of body hair. A 4-mm punch biopsy sent for histopathologic examination revealed dense, chronic, perifollicular inflammation affecting the mid and upper portions of the follicles, with loss of associated sebaceous glands. Involved hairs demonstrated vacuolar interface disruption of the basilar and epibasilar layers at the level of the isthmus and infundibulum, with prominent exocytosis of lymphocytes into the outer root sheath. There was no miniaturization, dermal mucin, or inflammation affecting the epidermis, arrector pili muscles, and eccrine glands (Figure 2).
A diagnosis of FFA was confirmed by these findings. Our patient was managed with intralesional triamcinolone acetonide (10mg/cc) injections, clobetasol 0.05% ointment BID, hydroxychloroquine 200 mg PO BID, and minoxidil 5 mg PO daily. Unfortunately, her alopecia did not stabilize with these measures.
FFA is a primary lymphocytic cicatricial alopecia that is currently regarded as a variant of lichen planopilaris. It is characterized by band-like frontotemporal hairline recession, often with associated eyebrow alopecia, perifollicular erythema, and scaling. Clinical findings are frequently accompanied by pruritus and burning of the affected scalp. Since it was first described in 1994,1 FFA has largely been viewed as an alopecia of post-menopausal Caucasian women. This archetype has been maintained by patient demographics of subsequent published case series.2,3 FFA may thus be underdiagnosed in black women, in whom traction alopecia, central centrifugal cicatricial alopecia, and androgenetic alopecia are assumed to be more common. Furthermore, FFA can manifest uniquely in black women, who may be premenopausal4,5 and asymptomatic4 at the time of presentation. Classic signs of FFA may be subtle or absent among black patients, as increased pigmentation may render erythema difficult to appreciate, while oils and hair care products may diminish the appearance of scale.
It is important for dermatologists to both recognize that FFA is not uncommon in the black population,4,5 and to acknowledge how it initially came to be regarded as a disease of post-menopausal white women. Several of the larger published series come from geographic areas that lack a substantial skin of color population.2,3 There are also socioeconomic factors to consider. One series comprised exclusively of Caucasian women found their patients to be more affluent, which was speculated to be a surrogate marker for an unknown risk factor associated with the development of FFA.3 What these authors did not discuss, however, is that affluence enables access to specialty medical care. Affluence affects insurance status, which has been shown to vary widely among racial groups.6 Insurance status in turn bears upon who has access to dermatologic care, and who is ultimately included in a case series.
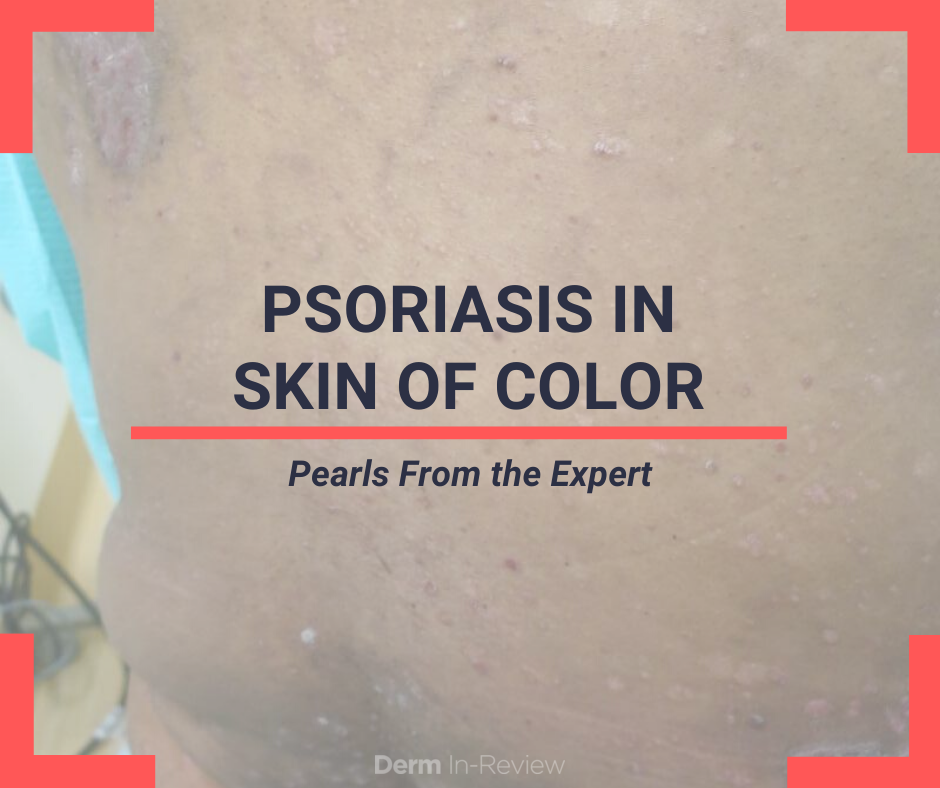
Andrew Alexis, MD, MPH, co-chair and co-founder of Skin of Color Update presented on Psoriasis in Skin of Color this past event.
Previously thought to be rare in patients of African ancestry, the prevalence of psoriasis is 1.6% in African Americans and 1.4% in Hispanics.
The talk, “Psoriasis: Distinct Clinical Features and Treatment Options of Psoriasis Patients of Color, ” was one of the top rated lectures of Skin of Color Update.
The lecture focused on the fundamentals of dermatology with an emphasis on several key characteristics.
During the lecture, Dr. Alexis presented a game of “Psoriasis or Not?” allowing the audience to guess if the Kodachrome was psoriasis. This illustrated the vast presentation of psoriasis and how papulosquamous disorders can be challenging to differentiate in skin of color.
To read more about this lecture and psoriasis in skin of color, visit the full article on Next Steps in Derm.
Purchase lectures like this one:
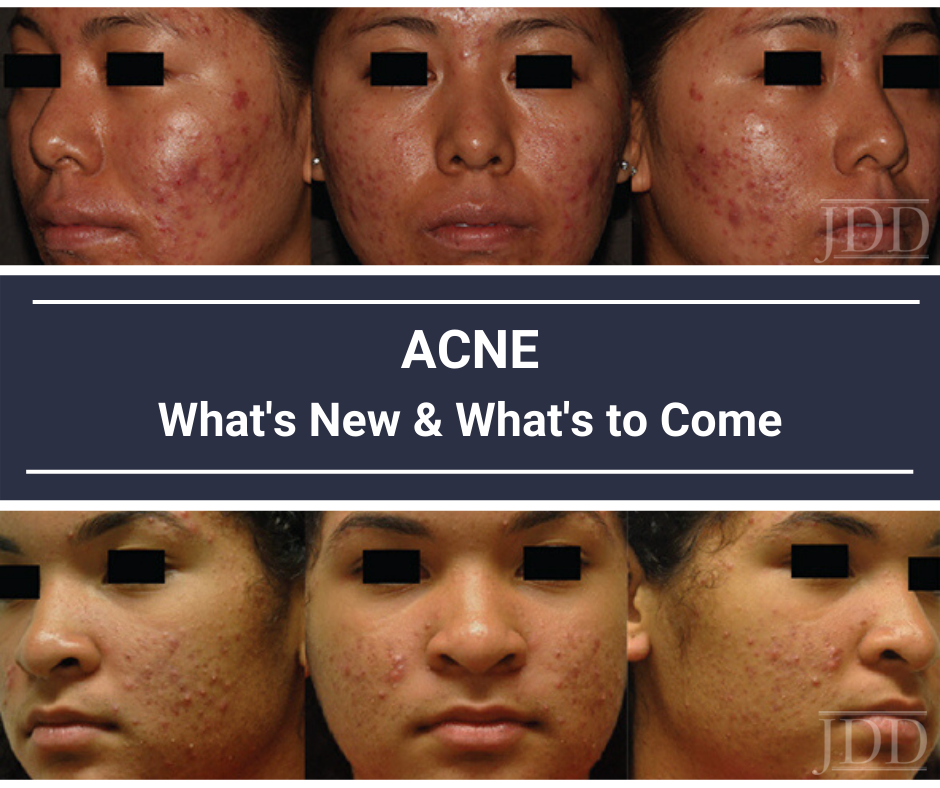
At Skin of Color Update 2019, our co-chair and co-founder, Andrew Alexis, MD, MPH gave a lecture on Acne: What’s New and What’s to Come? Our onsite correspondent, Kimberly Huerth, MD, M. Ed, provided the following recap of this is insightful session. The read the full article, please visit Next Steps in Derm website. Missed Skin of Color Update 2019? Purchase lectures like this on-demand.
By: Kimberly Huerth, MD, M. Ed
I still treat my acne twice daily with a whole cabinet full of various topicals. I’ve tried and failed doxycycline because it disrupts every single molecule of bacterial flora in my body. I’ve tried and failed spironolactone because I was the poster child for nearly all of its annoying and inconvenient side effects. I’ve tried and failed several OCPs because my body was a little too convinced by the estrogen and progesterone that it was actually pregnant, and decided to make me persistently sleepy and nauseous. I could put the 650-microsecond Nd:YAG that we have in clinic to use, but can’t bring myself to bother my co-rezzys (or myself) at the end of a long day seeing patients. And yes, I’ve already done a course of isotretinoin…two courses in fact. And no, I don’t have PCOS. So when I settled in to hear Dr. Andrew Alexis’s lecture on Acne in Skin of Color: What’s new and what’s to come?, I was excited for some new strategies with which to help my patients, and myself.
Dr. Alexis not only shared expert insights and strategies on how to optimize treatment for acne in skin of color (SOC) patients, but he also laid out an overview of some of the new and emerging acne treatments that we will presently be able to add to our armamentarium!
This article will provide an overview of the following:
But first, let me share a few of the “A-ha” moments that I experienced during Dr. Alexis’s lecture, in the hope that they will entice you to read on…
Missed Skin of Color Update 2019? Purchase lectures like this on-demand.

New York (Nov. 5, 2019) Skin of Color Update launches on-demand video package. Skin of Color Update, the largest CE event dedicated to trending evidence-based research and new practical pearls for treating skin types III – VI expands educational offerings to include on-demand videos.
The demand for skin of color dermatology education is greater than Skin of Color Update’s ability to accommodate onsite. Therefore, SanovaWorks has produced and launched a Best of Skin of Color Update video package. The video content is comprised of the highest attendee rated sessions of Skin of Color Update 2019. On-demand videos include top-rated faculty lectures in-sync with PPT slides with accompanying audio files.
On-demand Lectures include:
The video content focuses on expert techniques, real-life clinical cases and expert pearls immediately useful in the practice. For a video preview, click here.
Purchase the on-demand Best of Skin of Color Update video package and start learning from the experts today.

Each month the Journal of Drugs in Dermatology JDD Podcast discusses a current issue in dermatology. During the month of September, podcast host Dr. Adam Friedman sat down with Skin of Color Update 2019 co-chair and co-founder, Dr. Andrew Alexis, Chair of Dermatology at Mt. Sinai St. Lukes and Mount Sinai West to discuss misconceptions regarding the aesthetic skin of color consumer.
Dr. Angela Hou, PGY-3 dermatology resident at George Washington University School of Medicine and Health Sciences, shares key takeaways from Dr. Alexis’ JDD podcast titled ‘Capturing Consensus and Cutting Out misconceptions regarding the Aesthetic Skin of Color Consumer’.
Here is an excerpt recently published on our media partner, Next Steps in Dermatology.
Key Takeaways
To hear the JDD podcast, click here.
Purchase
During the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference, I had the pleasure of taking part in the Resident Career Development Mentorship Program (a program supported by an educational grant from Sun Pharmaceutical Industries, Inc.). and was paired with Dr. Andrew Alexis, Chair of Dermatology at Mount Sinai St. Luke’s and Mount Sinai West in New York City.
During a 45-minute working group session, Dr. Alexis covered three main themes: common dermatologic disorders with unique manifestations in skin of color, disorders that disproportionately affect patients of color and therapeutic nuances and unique treatment concerns in skin of color. Here are the main takeaways and pearls from this session.
Acne
Post-inflammatory hyperpigmentation is a major concern in patients of color and many times more bothersome than acne itself. It is important to use agents that will treat both acne and PIH. Retinoids can be very effective –tretinoin, tazarotene and adapalene have been shown effect for PIH. Azelaic acid can be a good add on for patients with PIH.
Dr. Alexis doesn’t use much hydroquinone for these patients – the macules left behind by acne are usually too small to avoid creating halos around the lesion. Chemical peels have been demonstrated to improve PIH in small studies. The risks are higher in skin of color, so it advisable to stick to superficial peeling agents. Avoiding irritation is essential since it can lead to more dyspigmentation.
Maximize tolerability – adapalene and low concentration tretinoin or tazarotene are a good starting point. Eliminate any irritating scrubs and other skincare products. Use noncomedogenic moisturizers concurrently.
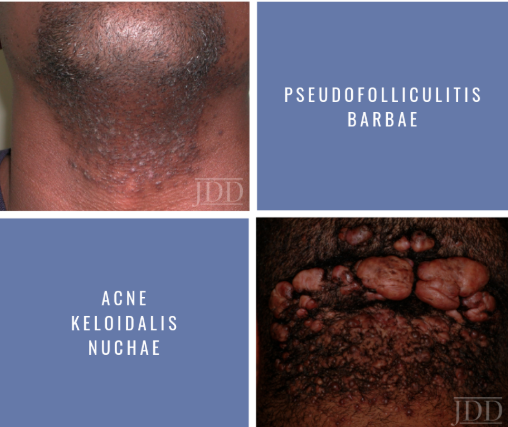
Pseudofolliculitis barbae
Findings consist of papules and prominent hyperpigmentation. This process can also trigger keloid formation. While more common in men, women with hirsutism may also develop PFB. It results from a foreign body reaction to hair reentering the dermis.
A very effective strategy is to discontinue shaving. You may have to write letters to some patients’ employers in order to excuse them from shaving (Dr. Alexis keeps a form letter on file in his practice).
Chemical depilatory agents are a decent option. Barium sulfide powder and calcium thioglycolate cream can be used every 2-4 days. However, they can cause irritant dermatitis. Some patients may also find success by modifying their shaving practices. Don’t assume your patients know how to shave – educate them. Electric clippers are a good option – have patients leave 0.5-1 mm stubble. Traditionally single blade manual razors have been recommended.
One study sought to quantify the impact of blade number on PFB – 90 African American men were assigned to shave with a different number of blades. There was no difference between any of the groups and everyone got better.
A small study showed decreased severity of PFB with daily shaving vs twice weekly shaving.
Dr. Alexis has a handout for patients with shaving instructions: before shaving use a mild cleanser and use a wash cloth in a circular motion to free hairs. Use clean and sharp razor, shaving in the direction of hair growth. Use topicals after such as clindamycin lotion or topical dapsone. Apply a topical retinoid nightly. Avoid pulling or plucking embedded hairs, shaving against the grain.

The medical education event focused on the dermatologic treatment of skin of color has a new name. Skin of Color Update, previously the Skin of Color Seminar Series, provides dermatologists with evidence-based research and practical pearls in treating skin of color, including patients with multiracial backgrounds.
“Just as the treatment of skin of color has evolved, this event has also evolved,” says Skin of Color Update co-chair and founding dermatologist Eliot Battle, MD. “Thanks to audience feedback, nearly all general sessions will have additional time for Q&A, making this year’s event the most interactive yet.”
Skin of Color Update will now be held annually in the fall. The 2019 event will be held September 7 and 8 at the Crowne Plaza Times Square in New York.
Skin of Color Update uses a didactic, case-based approach through lectures, hands-on-training and live demonstrations. Co-founding dermatologist Andrew Alexis, MD, also serves as an event co-chair. Common skin, hair and nail conditions in diverse populations will be covered. In addition, advanced treatment protocols for pigmentary and hair disorders will be shared during mini symposiums.
Sessions will address medical, surgical and cosmetic dermatology. New sessions include: