Source: Journal of Drugs in Dermatology
The recommendations are noted in the article, Considerations of Managing Lichen Planopilaris With Hydroxychloroquine During the COVID-19 Pandemic, will be available in the June print issue of the Journal of Drugs in Dermatology.
Chloroquine (CQ) and hydroxychloroquine (HCQ), two well-known drugs among dermatologists, have shown their efficacy in the inhibition of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) replication.1,2 HCQ is found to possess a better clinical safety profile, more potency, and fewer drug–drug interactions compared to chloroquine.3 HCQ has been reported to exert efficacy in the inhibition of SARS-CoV-2 in vitro replication through diverse mechanisms. First, it interferes with the glycosylation of angiotensin-converting enzyme 2 (ACE2), resulting in a subsequent reduction in the binding efficacy between ACE2 on host cells and the SARS-CoV-2 spike protein. Second, it blocks the fusion of the virus to the host cell. Finally, it suppresses the “cytokine storm” accountable for the disease progression to acute respiratory distress syndrome (ARDS). Although studies are underway to confirm the in vivo effectiveness of HCQ in the SARS-CoV-2 infection, promising primary results have led to a shortage of the drug for dermatologic purposes, which is a real concern in the current pandemic.1
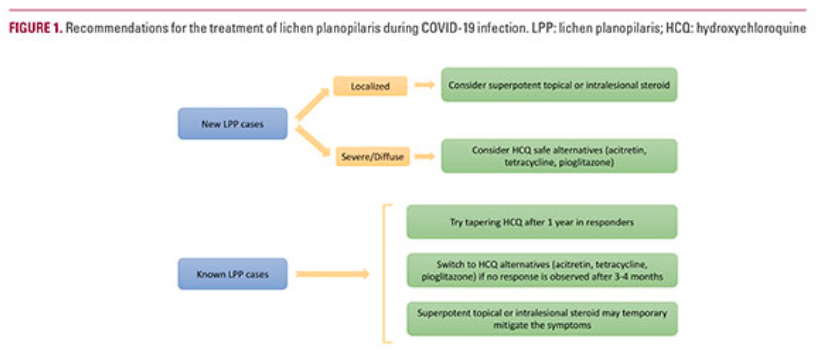
While we are amid a pandemic with the possible shortage of HCQ, dermatologists should be reminded that:
- The anti-inflammatory effect of HCQ may improve the clinical signs of LPP; however, administration of this drug is insufficient to prevent the subclinical disease progression.9 Dermatologists may discontinue the use of HCQ in responders after 1 year with monitoring the patients for recurrence or relapse.5
- Topical and intralesional super potent corticosteroids are recommended as the first-line treatment in localized LPP.4
- Oral cyclosporine followed by systemic corticosteroid may be the most effective medications in LPP; however, disease relapse may be detected.10 Mycophenolate mofetil has a more favorable safety profile compared to cyclosporine11 but the immunosuppressive nature of these medications necessitates extreme caution toward their administration during COVID-19 pandemic.12
- Acitretin (25 mg/day) may be an appropriate alternative since it has shown improvement in 66% of patients.7
- Pioglitazone (hypoglycemic drug, 15–30 mg/day) has shown some efficacy in the treatment of LPP and can be considered as an alternative to HCQ.4
- Tetracyclines antibiotics can also be considered as an alternative due to favorable outcomes in previous studies.13
