Source: JDD Online
The following is an excerpt from the Journal of Drugs in Dermatology article, Long-Term Benefits of Daily Photo-Protection With a Broad-Spectrum Sunscreen in United States Hispanic Female Population.
Introduction
The demographics of the United states are evolving with a large increase in racial and ethnic diversity driven by international migration of Hispanic, African, and Asian populations leading to a minority-majority shift in ~2050 towards persons of color (Fitzpatrick III, IV, V, and VI).1 Specifically, the Hispanic population is projected to be among the fastest growing population in the US, projected to increase from 55 million in 2014 to 119 million in 2060, a change of +115%.1
Subjects with skin of color are heterogeneous with multiple shades and tones and different reactions to intrinsic and extrinsic aging factors due to structural and physiologic differences.2,3 Skin of color individuals have fewer visible signs of aging (deep wrinkles, fine lines, rough surface texture, and sun spots). However, darker skin tones are more susceptible to certain skin conditions including post-inflammatory hyperpigmentation (may occur after acne, eczema, injury, laceration, melasma, post-inflammatory hypopigmentation, pityriasis alba (round, light patches covered with fine scales), dry or “ashy” skin, dermatosis papulosa nigra, and/or greater risk of keloid development.2,3 The incidence of skin cancer among US Hispanics has also increased 1.3% annually from 1992 to 2008.4
Photodamage is characterized histologically by degeneration of the connective tissue and abnormalities in keratinocytes and melanocytes. Clinically, it manifests primarily with wrinkles, dyschromia, texture changes, and, in more severe cases skin cancer.5 Formulations containing broad spectrum sunscreens against both UVA and UVB play an essential role in the prevention of photodamage and UV-induced skin cancers.6,7,8 However, the majority of clinical research on photoprotection has been conducted on subjects with Fitzpatrick types I to III skin and have reported improvements in signs associated with skin aging and texture.9,10 Verschoore et al was the first to conduct a short-term clinical study in India with Phototype IV and VI subjects, and provided first evidence on the effectiveness of daily sunscreen use on skin tone and radiance.11 Similar benefits were observed in an 8-week study in US.12
Although sun protection is highly recommended by dermatologists for skin cancer risk-reduction and the prevention of premature aging or pigmentary disorders, adherence to the recommendations is not commonly observed among US Hispanics.13 Moreover, a large number of US Hispanics reside in areas with high UV index with a high degree of sun seeking behavior. Among Hispanic adults who report engaging in sun protection, they do so mostly by staying in the shade (53.7%) rather than use of sunscreen (32.3%) or wearing sun protective clothes (18.1%); while 36.7% of the subjects surveyed indicated that they never use sunscreen.14,15 There are sociodemographic factors that contribute to the adherence to safe sun behaviour such as education, age, and gender, etc, therefore there is a need to raise awareness of skin cancer risks, advocate for preventive measures and educate on benefits of sunscreen and sun protection among US Hispanics.16
The benefits of topical agents for reversal of sun damage has been well established. Use of retinoic acid and its derivatives or other drugs to reverse and improve sun damaged skin has been demonstrated in many studies.17,18 Long-term sunscreenuse along with other topical agents have also been shown to prevent photodamage and hyperpigmentation in fair-skinned subjects.19 For effective photoprotection, sunscreen products containing both SPF and PPD are essential to battle the harmful UVB (skin cancer risks) and UVA (photo-aging risks).20 Daily use of a broad-spectrum sunscreen (SPF 30) over a one-year period has also been demonstrated to improve clinical parameters of photodamage in phototype I-III subjects.10 However, a comprehensive long-term sunscreen use study in skin of color is lacking. Therefore, this study was designed to assess the benefits of sunscreen of SPF30/PPD 20 in Hispanic women of Fitzpatrick skin types IV and V over 12 months in comparison to a real-life observational group with subjects who did not use sunscreen regularly.
Read Full Article….
Discussions and Conclusions
Effective photoprotection is critical for healthy skin, in preventing skin cancers, reducing photodamage, and improving aesthetic appearance. A broad spectrum sunscreen protecting against both UVA and UVB irradiation is essential. Protecting against the UVA spectrum needs special attention, especially under daily diffused exposure, as UVA is more penetrating and less affected by seasonality and impacts photoaging and skin oxidative stress.22 It has been reported that in order to receive effective photoprotection on skin, a PPD value of 18 is desired.20 In this study, the investigational product with SPF 30/PPD 20 is considered sufficient for daily activity without prolonged direct sun exposure when applied properly. Concerning skin of color population, the use of sunscreen is lower than in Caucasians despite high prevalence of sun-related pigmentary disorders and rising rates of cutaneous cancers.4 This study provides strong evidence to educate and advocate for daily use of a proper sunscreen product for populations with high phototype skin.
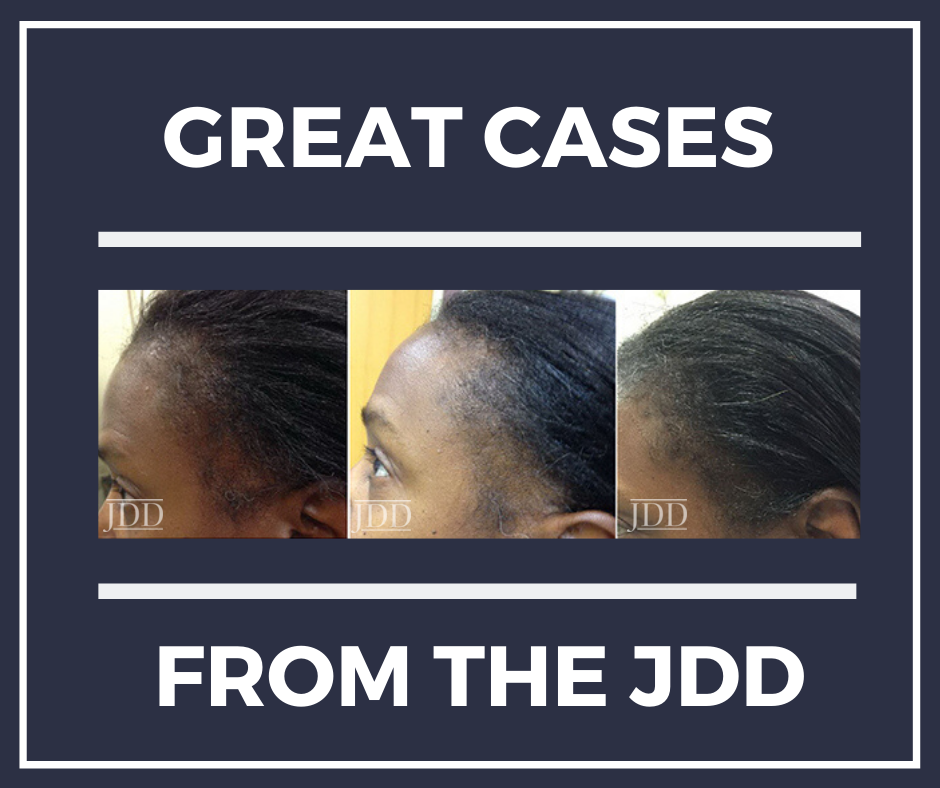
The clinical evaluation demonstrated significant visible improvement in sunscreen group starting from 3 months and progressive increased over time. Benefits on multiple facial areas and body sites were visible (upper, mid- and lower face, neck, and hands), not only on pigmentary-related concerns (skin tone evenness, overall hyperpigmentation, dark spots, and blotchiness), but also on aging parameters such as fine lines, skin texture, and overall skin quality. This suggests that beyond the preventative benefits, long-term persistent use of a proper sunscreen may also allow the photodamaged skin to self-heal and repair over time.
Histological observations further supported the clinical findings. The observation that the real-life group had higher tendency for pigmentation incontinence is of strong research interest. It has been reported that UV irradiation can destabilize and damage the dermal-epidermal junction (DEJ), which facilitates the entrapment of melanin in the dermis.23 The dermal melanin is extremely difficult to remove, often resulting in stubborn hyperpigmentation.24 This is especially important for skin of color population in whom dermal hyperpigmentation lesions are common and can be worsened with excessive sun exposure. This study provides the first evidence that effective daily photoprotection can be a strategy to prevent dermal melanin formation by protecting the DEJ. A larger sample size study with DEJ biomarkers will help to further elucidate this hypothesis. Infiltration of CD68-positive Macrophages is a hallmark of the inflammatory response after UV irradiation. In the dermis, 2 out of 3 of the real-life biopsy samples showed significant increase in CD68 positive macrophage cells at 12 months compared to baseline, while such change was not observed in the sunscreen group. This suggests the potential preventative benefits of sunscreen in subclinical skin inflammation induced by chronic exposure to UV. In all of the histological evaluations, thegeographical location in which the study was conducted (Los Angeles versus Washington, DC) was not a strong contributing factor to any of the observed differences. However, the histological findings in this study are limited by the small number of biopsies obtained.
In summary, this 12-month study on long-term persistent use of an SPF30/PPD20 sunscreen on phototype IV and V subjects demonstrated significant improvement in skin quality and improvement in skin color and photoaging parameters. To our knowledge, this is the first study of this kind in skin of color and Hispanic population. This study confirms that effective sunscreen use is not only protective and beneficial for light skin population but is also critical in improving skin condition for skin of color patients. Overall, the study demonstrates that daily use of sunscreen can protect skin from photo related damage and even reverse some of the photo-damage that has already occurred in skin. In addition to previous studies that demonstrated the photo-protective properties of sunscreen use in normal and diseased skin states7,8,9,10 and in view of the fact that good photoprotection behaviors are not common among Hispanics,14,15,16 studies of this type can help educate and stress the importance of daily use of sunscreen and other sun protection behaviors in Hispanic and other skin of color populations.
Read Full Article….