NEW YORK, Jan. 25, 2022 /PRNewswire/ — WebMD Health Corp., an Internet Brands company and a leader in health information services for physicians, other healthcare professionals and consumers, today announced that it has acquired SanovaWorks, a global multiplatform company focused on delivering targeted educational offerings and learning solutions for dermatologists.
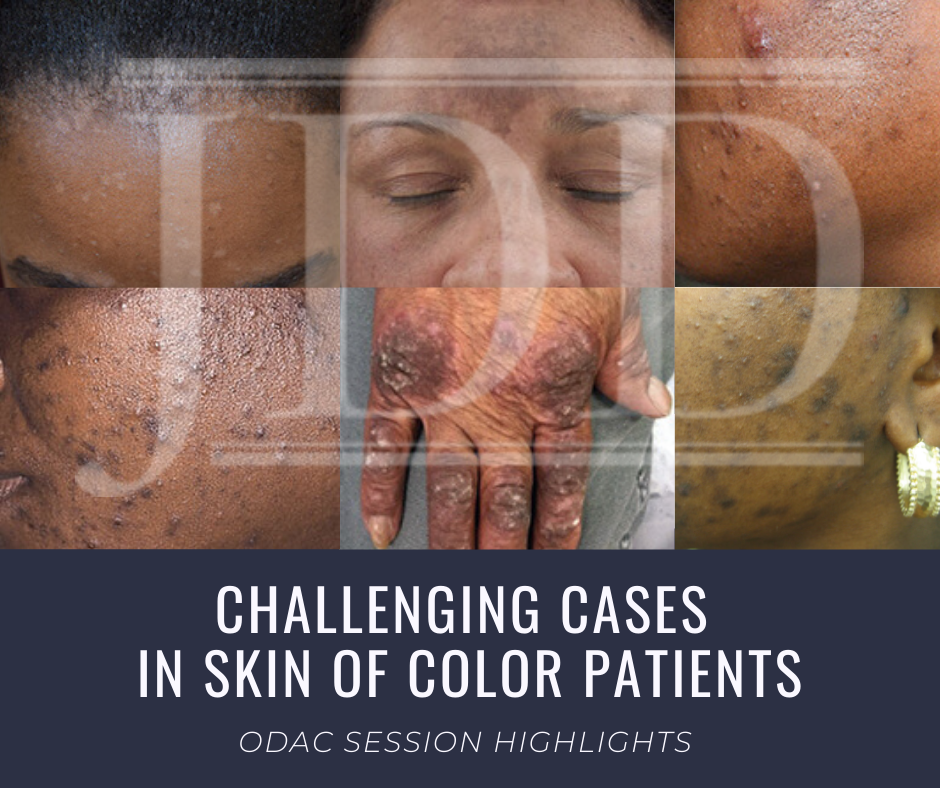
Sanovaworks hosts leading medical conferences ODAC Dermatology, Aesthetics and Surgical and Skin of Color and offers web-based learning tools, publications such as Journal of Drugs in Dermatology (JDD) and virtual webinar and podcast series. In addition, SanovaWorks offers the online and audio-format Derm in Review, a board certification and recertification course.
The acquisition builds on the core competencies of WebMD’s MedscapeLIVE, Medscape’s market leading experiential business providing impactful in-person and virtual opportunities for healthcare professionals (HCPs) to congregate, learn and share. MedscapeLIVE offers proprietary live conferences, peer-to-peer webinars, symposia and various other educational engagement programs.
“The addition of SanovaWorks deepens WebMD’s commitment to providing high-quality, engaging experiences for HCPs with an expanded offering to dermatologists, one of our largest professional communities,” said Ann Bilyew, Internet Brands Senior Vice President, Health and WebMD Group General Manager, Provider Services. “With SanovaWorks, we build on MedscapeLIVE’s innovative learning solutions with expansive and relevant content that supports dermatologists throughout their careers, while providing additional opportunities to reach this important audience for sponsors and supporters.”
“SanovaWorks shares WebMD’s core mission to continually meet the educational needs of clinicians with the information and content they need, when and where they need it,” said Shelley Tanner, CEO of Sanovaworks. “The extensive reach of MedscapeLIVE with dermatology professionals worldwide enables us to have an even greater impact, particularly as their need for timely, relevant learnings grows.”
Terms of the acquisition were not disclosed.
About SanovaWorks
SanovaWorks is a healthcare communications company with more than 20 years of experience in the creation and dissemination of educational resources in dermatology, aesthetics and beyond. Reaching over 100,000 worldwide dermatology professionals monthly, SanovaWorks is a trusted healthcare communication source that produces the Journal of Drugs in Dermatology (JDD), ODAC Dermatology, Aesthetic and Surgical Conference, Skin of Color Update, Next Steps in Dermatology, Dermatology In-Review and the newly released Atlas in Dermatology. For more information, please visit sanovaworks.com.
About WebMD Health Corp.
WebMD, an Internet Brands company, is at the heart of the digital health revolution that is transforming the healthcare experience for consumers, patients, healthcare professionals, employers, health plans and health systems. Through public and private online portals, mobile platforms, and health-focused publications, WebMD delivers leading-edge content and digital services that enable and improve decision-making, support and motivate health actions, streamline and simplify the healthcare journey, and improve patient care.
The WebMD Health Network includes WebMD Health, Medscape, Jobson Healthcare Information, MediQuality, Frontline, Vitals Consumer Services, Aptus Health, Krames, PulsePoint, The Wellness Network, MedicineNet, eMedicineHealth, RxList, OnHealth, Medscape Education, and other owned WebMD sites. WebMD®, Medscape®, CME Circle®, Medpulse®, eMedicine®, MedicineNet®, theheart.org® and RxList® are among the trademarks of WebMD Health Corp. or its subsidiaries.
About Internet Brands
Headquartered in El Segundo, Calif, Internet Brands® is a fully integrated online media and software services organization focused on four high-value vertical categories: Health, Automotive, Legal, and Home/Travel. The company’s award-winning consumer websites lead their categories and serve more than 250 million monthly visitors, while a full range of web presence offerings has established deep, long-term relationships with SMB and enterprise clients. Internet Brands’ powerful, proprietary operating platform provides the flexibility and scalability to fuel the company’s continued growth. Internet Brands is a portfolio company of KKR and Temasek. For more information, please visit www.internetbrands.com.
SOURCE WebMD Health Corp. via PR News Wire