During the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference, I had the pleasure of taking part in the Resident Career Development Mentorship Program (a program supported by an educational grant from Sun Pharmaceutical Industries, Inc.). and was paired with Dr. Andrew Alexis, Chair of Dermatology at Mount Sinai St. Luke’s and Mount Sinai West in New York City.
During a 45-minute working group session, Dr. Alexis covered three main themes: common dermatologic disorders with unique manifestations in skin of color, disorders that disproportionately affect patients of color and therapeutic nuances and unique treatment concerns in skin of color. Here are the main takeaways and pearls from this session.
Common Disorders With Unique Manifestations
Acne
Post-inflammatory hyperpigmentation is a major concern in patients of color and many times more bothersome than acne itself. It is important to use agents that will treat both acne and PIH. Retinoids can be very effective –tretinoin, tazarotene and adapalene have been shown effect for PIH. Azelaic acid can be a good add on for patients with PIH.
Dr. Alexis doesn’t use much hydroquinone for these patients – the macules left behind by acne are usually too small to avoid creating halos around the lesion. Chemical peels have been demonstrated to improve PIH in small studies. The risks are higher in skin of color, so it advisable to stick to superficial peeling agents. Avoiding irritation is essential since it can lead to more dyspigmentation.
Maximize tolerability – adapalene and low concentration tretinoin or tazarotene are a good starting point. Eliminate any irritating scrubs and other skincare products. Use noncomedogenic moisturizers concurrently.
Disorders That Disproportionately Affect Patients of Color
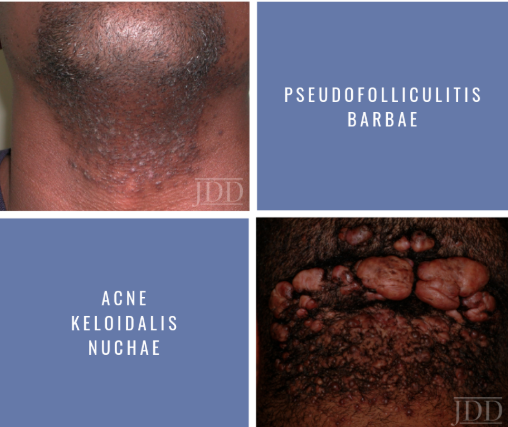
Pseudofolliculitis barbae
Findings consist of papules and prominent hyperpigmentation. This process can also trigger keloid formation. While more common in men, women with hirsutism may also develop PFB. It results from a foreign body reaction to hair reentering the dermis.
A very effective strategy is to discontinue shaving. You may have to write letters to some patients’ employers in order to excuse them from shaving (Dr. Alexis keeps a form letter on file in his practice).
Chemical depilatory agents are a decent option. Barium sulfide powder and calcium thioglycolate cream can be used every 2-4 days. However, they can cause irritant dermatitis. Some patients may also find success by modifying their shaving practices. Don’t assume your patients know how to shave – educate them. Electric clippers are a good option – have patients leave 0.5-1 mm stubble. Traditionally single blade manual razors have been recommended.
One study sought to quantify the impact of blade number on PFB – 90 African American men were assigned to shave with a different number of blades. There was no difference between any of the groups and everyone got better.
A small study showed decreased severity of PFB with daily shaving vs twice weekly shaving.
Dr. Alexis has a handout for patients with shaving instructions: before shaving use a mild cleanser and use a wash cloth in a circular motion to free hairs. Use clean and sharp razor, shaving in the direction of hair growth. Use topicals after such as clindamycin lotion or topical dapsone. Apply a topical retinoid nightly. Avoid pulling or plucking embedded hairs, shaving against the grain.