Andrew F. Alexis, MD, MPH
Eliot F. Battle, MD
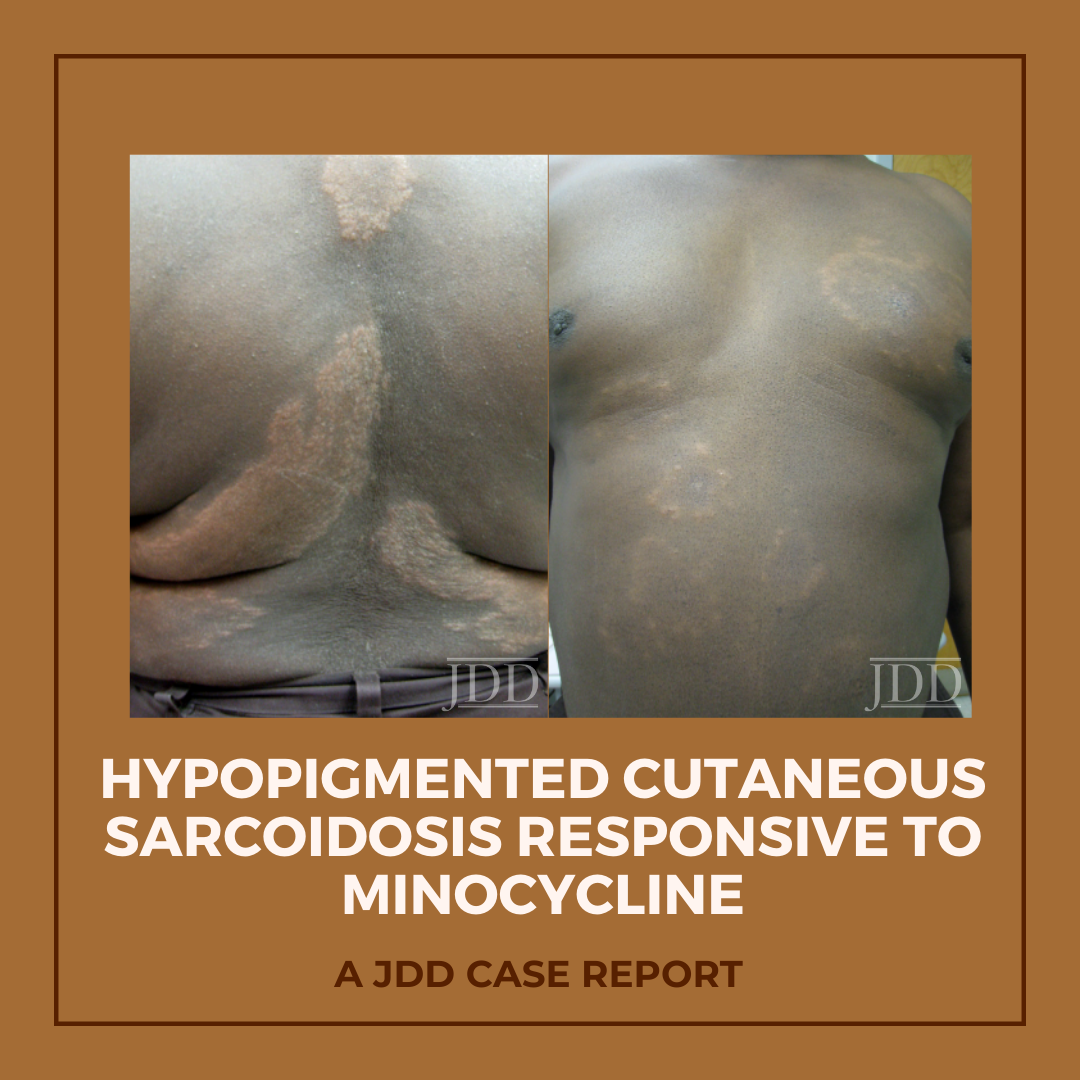
Hypopigmented patches and plaques are a rare presentation of cutaneous sarcoidosis. JDD authors describe a case of generalized hypopigmented cutaneous sarcoidosis that showed good response to minocycline therapy.

FIGURE 1. Hypopigmented plaques over the back.

FIGURE 2. Hypopigmented annular plaques of papules on the abdomen.
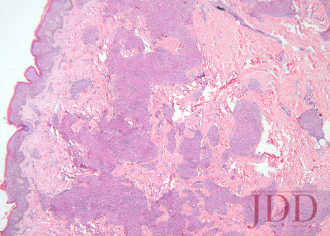
FIGURE 3. Hematoxylin and eosin stain of a left arm skin biopsy show-ing dermal granulomatous inflammation.
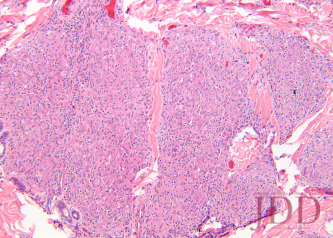
FIGURE 4. Hematoxylin and eosin stain of a left arm skin biopsy at higher magnification demonstrating well-formed naked granulomas.

FIGURE 5. Flattening and repigmentation of plaques on the back after treatment with minocycline.

FIGURE 6. Repigmentation of annuli on the anterior trunk after treat-ment with minocycline.
The skin is one of myriad organs potentially affected by sarcoidosis, a multisystem idiopathic disorder characterized histologically by infiltration of noncaseating granulomas. Cutaneous manifestations of sarcoidosis are protean, including papules and plaques of various morphology and distribution, subcutaneous nodules, pruritus, ichthyosis, erythroderma, ulceration, verrucosis, nail disease, and infiltrative scars.1 In the United States, sarcoidosis is more common in African-Americans than in other ethnic groups, and cutaneous manifestations in individuals of African descent are more likely to be atypical.2
Minocycline as monotherapy was efficacious for the treatment of chronic cutaneous sarcoidosis in an open observational study of 12 patients by Bachelez et al.17 The cutaneous manifestations of patients in the Bachelez group included classic plaques, papulonodules, subcutaneous nodules, and lupus pernio. Ten of 12 patients completely or partially responded to treatment, which was generally well tolerated except for drug hypersensitivity syndrome in one patient with a history of other autoimmune diseases. Park et al later reported a patient with cutaneous, lacrimal gland, pulmonary, and ocular (choroidal) sarcoidosis that responded to minocycline.18
Originally published in the Journal of Drugs in Dermatology in April 2012.
Schmitt, C. E., Fabi, S. G., Kukreja, T., & Feinberg, J. S. (2012). Hypopigmented cutaneous sarcoidosis responsive to minocycline. Journal of drugs in dermatology: JDD, 11(3), 385-389. https://jddonline.com/articles/dermatology/S1545961612P0385X
Content and images republished with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
The Journal of Drugs in Dermatology is available complimentary to US dermatologists, US dermatology residents, and US dermatology NP/PA. Create an account on JDDonline.com and access over 15 years of PubMed/MEDLINE archived content.
Did you enjoy this case report? You can find more here.
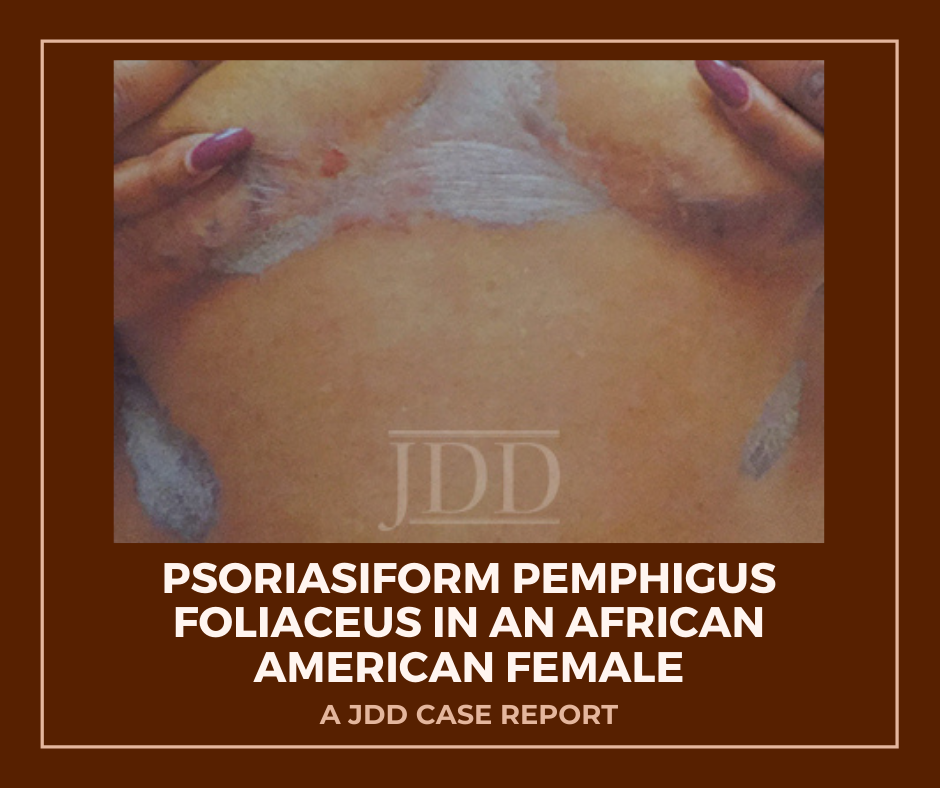
JDD authors document and highlight this atypical psoriasiform presentation of Pemphigus Foliaceus in a patient with skin of color to raise awareness and improve diagnosis and outcomes.
A 50-year-old African-American woman presented to the dermatology clinic with a pruritic eruption of 3 years’ duration that began as discrete plaques on the inframammary folds and subsequently spread towards the mid-chest, ears, back, elbows, knees, and scalp. Past treatments by other clinicians included clotrimazole cream and a topical corticosteroid of unknown potency without significant improvement. She denied any new medications and was taking aspirin, divalproex, mirtazapine, cetirizine, venlafaxine, atorvastatin, and omeprazole.
On clinical examination, the patient had well-demarcated, pink, atrophic plaques and superficial erosions over the inframammary folds and mid-chest (Figures 1). She also had well-demarcated, hyperpigmented, hyperkeratotic scaly plaques over the abdomen, suprapubic region, elbows, knees, and back with sporadic small superficial blisters (Figure 2). Complete blood count, complete metabolic panel, rheumatoid factor, and antinuclear antibody were within normal limits. Rapid plasma reagin test was negative. Erythrocyte sedimentation rate was elevated at 54 millimeter/hour (reference range 0-22 millimeter/hour). A punch biopsy of the right abdomen was performed and revealed psoriasiform epidermal hyperplasia, focal parakeratosis, and acantholysis throughout the superficial spinous and granular layers (Figure 3). Only a sparse inflammatory infiltrate was present in the underlying dermis. These clinical and histological findings supported the diagnosis of pemphigus foliaceus (PF). Patient was started on 50 mg oral dapsone daily.
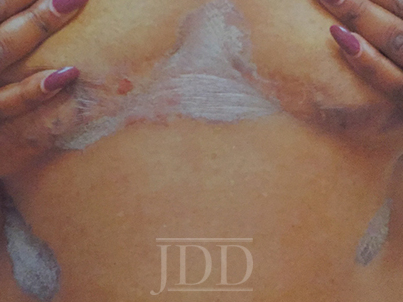
FIGURE 1. Well-demarcated, scaly plaques over the mid-chest and inframammary folds, with a single superficial erosion on the right medial chest.

FIGURE 2. A plaque from the abdomen demonstrates “corn flake-like” scale.
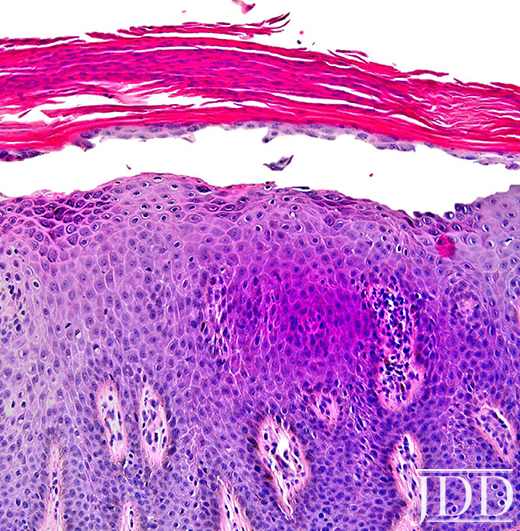
FIGURE 3. Composite photomicrograph, hematoxylin, and eosin, original magnification x200.
Herein, we present a case of Pemphigus Foliaceus with a psoriasiform clinical presentation in an African-American patient. PF is an autoimmune skin disease caused by antibodies against the desmosomal glycoprotein, desmoglein 1.¹ Desmogleins, members of the cadherin family, serve to anchor epidermal desmosomes between adjacent keratinocytes and assist in epithelial differentiation.² Antibodies targeting desmoglein 1 result in acantholysis in the upper epidermis with limited separation in the basal layers and minimal mucosal involvement as desmoglein 1 is primarily expressed in the granular layer of the non-mucosal epidermis.¹ Patients present with scaly plaques on an erythematous base and fragile shallow blisters which are infrequently found intact; rarely, the condition can progress to exfoliative erythroderma.1,3 Initially, PF usually presents on the trunk, face, or scalp, but may subsequently involve other regions of the skin.1 Diagnosis may be confirmed with biopsy and direct immunofluorescence with intercellular IgG and C3 limited to the upper epidermis. Treatment includes oral and topical steroids, azathioprine, dapsone, and rituximab. The differential diagnosis for PF may include systemic lupus erythematosus, bullous impetigo, psoriasis, and seborrheic keratosis depending on the presentation.1
Physical exam findings in this patient were suggestive of PF due to the presence of superficial secondary erosions and “corn flake-like” scales, but psoriasis was included in the differential diagnosis due to the presence of discrete plaques with an erythematous border. PF is a relatively rare condition with a prevalence of less than 1 case per 100,000 and is about 5 to 10 times less common than pemphigus vulgaris.4 In contrast, psoriasis impacts approximately 2-4% of people in the United States.5 An endemic form of PF, fogo selvagem, has been reported in Brazil, Colombia, Peru, and Tunisia, while pemphigus vulgaris is more common in Mediterranean and Ashkenazi Jewish populations.4
We hypothesize that patients with psoriasiform presentations of PF may be misdiagnosed with plaque psoriasis. One author (JJ) has previous significant clinical experience with patients with skin of color and has seen other skin of color patients present with a psoriasiform manifestation of PF. PF and psoriasis share similar treatments including topical corticosteroids and immunosuppressants, and this may lead to underreporting of PF with psoriasiform manifestations. It is important to distinguish between these findings as there is evidence that ultraviolet light, a common treatment for psoriasis, may exacerbate PF.6,7 We performed a search of the published literature and identified one article that describes three patients with pemphigus erythematosus, a variant of PF, which was misdiagnosed as psoriasis.8 No identified articles described cases of PF with a psoriasiform presentation in patients with skin of color. We document and highlight this atypical psoriasiform presentation of PF in a patient with skin of color to raise awareness and improve diagnosis and patient outcomes.
Originally published in the Journal of Drugs in Dermatology in April 2018.
Evan Austin BS, Jillian W. Millsop MD, Haines Ely MD, Jared Jagdeo MD MS, and Joshua M. Schulman MD (2018). Psoriasiform Pemphigus Foliaceus in an African American Female: An Important Clinical Manifestation. Journal of Drugs in Dermatology, 17(14), 471-473. https://jddonline.com/articles/dermatology/S1545961618P0471X
Content and images republished with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
The Journal of Drugs in Dermatology is available complimentary to US dermatologists, US dermatology residents, and US dermatology NP/PA. Create an account on JDDonline.com and access over 15 years of PubMed/MEDLINE archived content.
Did you enjoy this case report? You can find more here.