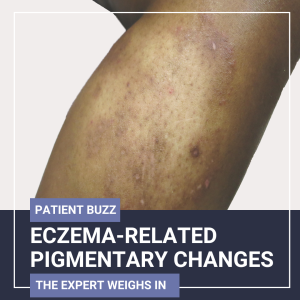
Our sister conference, the ODAC Dermatology Conference, also offers sessions that address the dermatologic treatment of patients with skin of color. At ODAC 2025, Pooja Sodha, MD, associate professor of dermatology and director of laser and cosmetic dermatology at GWU School of Medicine and Health Sciences, presented a comprehensive, case-based review of post-inflammatory hyperpigmentation and post-inflammatory hypopigmentation. In the session, Dr. Sodha highlighted diagnostic techniques and a stepwise, multimodal treatment approach.
Post-Inflammatory Hyperpigmentation (PIH)
PIH results from inflammation-induced melanocyte activation, often triggered by trauma, medications, or autoimmune processes. Dr. Sodha emphasized differentiating PIH from mimickers, such as melasma and drug-induced pigmentation. Diagnosis relies on clinical history and visual examination, aided by Wood’s lamp, polarized photography, and reflectance confocal microscopy for depth assessment and histologic correlation.
Treatment strategies target both the inflammatory trigger and melanin production pathway, using:
- Hydroquinone and mild topical steroids for short-term pigment inhibition.
- Timolol gel to reduce early post-inflammatory erythema.
- 2MNG with niacinamide to safely block melanosome transfer.
- Laser modalities, such as 595-nm pulsed dye laser and 1927-nm diode laser, for vascular and epidermal pigment targets.
- Topical antioxidants (silymarin, vitamin C, ferulic acid) and retinoids (tazarotene) to combat oxidative stress.
- Laser-assisted drug delivery (LADD) with tranexamic acid to enhance pigment reduction.
- Cysteamine cream as a long-term alternative to hydroquinone.
- 1064-nm picosecond laser (Pico-toning) for dermal pigment shattering and remodeling.
Dr. Sodha underscored the vascular component of PIH, linking elevated VEGF levels to increased melanogenesis and advocating early treatment of erythema.
Post-Inflammatory Hypopigmentation (PIHpo)
PIHpo can arise after laser-induced injury, especially with excessive fluence or improper wavelength selection.
Management aims to restore melanocyte function using:
- Topical clobetasol, transitioning to tacrolimus ointment for long-term use.
- Bimatoprost to stimulate melanocyte migration and melanin synthesis.
- 1550-nm erbium-doped fractional laser with LADD of bimatoprost for repigmentation.
- Excimer laser therapy, offering up to 70% improvement, though requiring multiple sessions.
Key Takeaways
- A deep understanding of inflammation’s impact on melanocytes is essential for both PIH and PIHpo.
- Early intervention, combination therapy, and individualized treatment based on skin type and pigmentation depth yield the best outcomes.
- Laser-assisted drug delivery enhances topical efficacy.
- Patient education on treatment duration and session expectations is vital for success.
This session summary was written by Dr. Kala Hurst and published on Next Steps in Derm.