Please take a moment to acknowledge and thank our gracious supporter, Pfizer, by visiting their sponsor page on the Skin of Color Update 2021 Virtual Platform and their website below
Please take a moment to acknowledge and thank our gracious supporter, Abbvie, by visiting their sponsor page on the Skin of Color Update 2021 Virtual Platform and their website below.

AbbVie’s mission is to discover and deliver innovative medicines that solve serious health issues today and address the medical challenges of tomorrow. We strive to have a remarkable impact on people’s lives across several key therapeutic areas: immunology, oncology, neuroscience, eye care, virology, women’s health and gastroenterology, in addition to products and services across our Allergan Aesthetics portfolio.



Please take a moment to acknowledge and thank our gracious supporter, Scientis, by visiting their sponsor page on the Skin of Color Update 2021 Virtual Platform and their website below.

SanovaWorks has developed a partnership with and in support of Comprehensive Medical Mentoring Program. We are happy to announce that SanovaWorks will match the CMMP Medical Student Grant fund, which was started to help medical students from underrepresented populations with residency preparation expenses. This matching donation will ensure that more students are able to benefit from the grant. We join other partners in support of CMMP’s efforts of mentoring students, promoting diversity in medicine, and giving back to the communities.
READ MORE ABOUT CMMP’S PARTNERSHIPS
Medical Students, Grants are Now Available for Residency Expenses
Comprehensive Medical Mentoring Program (CMMP) is aware that applying to residency can be a daunting process which can also become more stressful given the associated expenses that come with it.
CMMP is providing grants up to $1,000 for rising 4th-year minority medical students as they are preparing for away rotations and residency applications.
IF YOU ARE
-
- a rising 4th-year medical school student, and
- applying for residency for the 2022-2023 academic year, and
- a member of an underrepresented group in medicine,
SUBMIT your application today!
The application deadline is May 15, 2021
Apply Today: https://sanovaworks.com/CMMP-medical-student-grant
JOIN US
SanovaWorks joins institutions that include George Washington University School of Medicine and Health Sciences, Howard University Hospital, Department of Dermatology, Georgetown University School of Medicine, and many others in support of CMMP.
Do you or an organization you know want to add your support to the Medical Student Grant Fund?
Contact Dr. Lauren Payne to add your company’s name to the partnership list: https://www.cmmpmed.org/contact-us/

Andrew F. Alexis, MD, MPH
Eliot F. Battle, MD
Source: Next Steps in Derm
Can you improve your culturally-competent hair loss consultation? Would you like to grow your toolbox for comprehensive alopecia treatment? If so, you are in the right place!
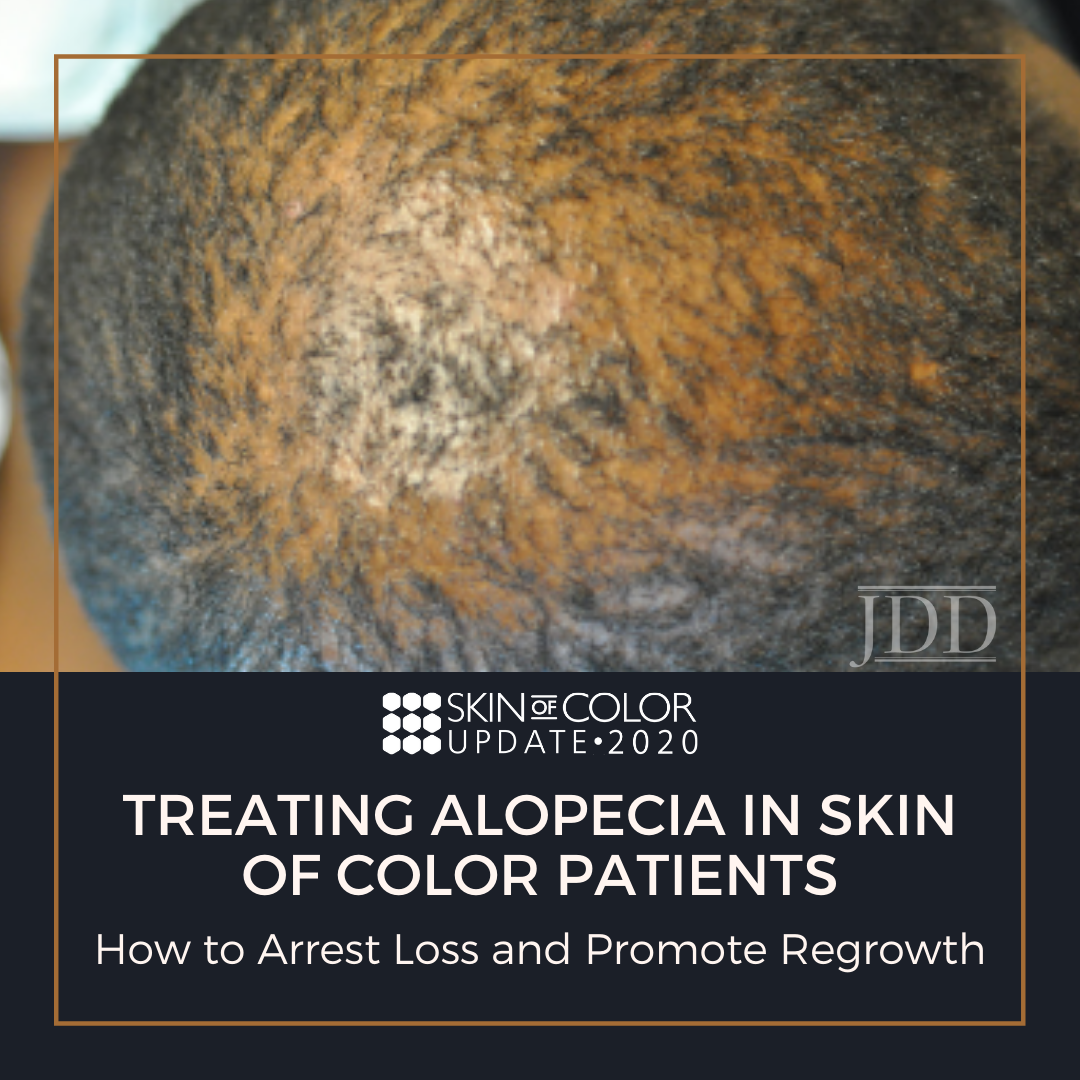
Hair loss is a frequent concern for patients visiting the dermatologist, especially in patients with pigmented skin types. Kinky or coiled hair has an innate fragility that makes African Americans especially prone to hair loss concerns. At the 2020 Skin of Color Virtual Update, Dr. Susan Taylor discussed Conventional Treatment Approaches for Hair & Scalp Disorders in Skin of Color Patients. Dr. Taylor advised how to have a culturally competent hair loss consultation, reviewed common patterns of hair loss, and highlighted comprehensive treatment of multifactorial causes of alopecia.
Before we get into therapeutic strategies for alopecia, let’s highlight important considerations to institute an effective treatment plan:
- Understand common ethnic hairstyles and practices
- Recognize the impact of hair and scalp disorders
- Clearly identify the problem and obtain a thorough history, including details regarding hair care practices, products used, and symptoms
- Complete physical examination and consider scalp biopsy
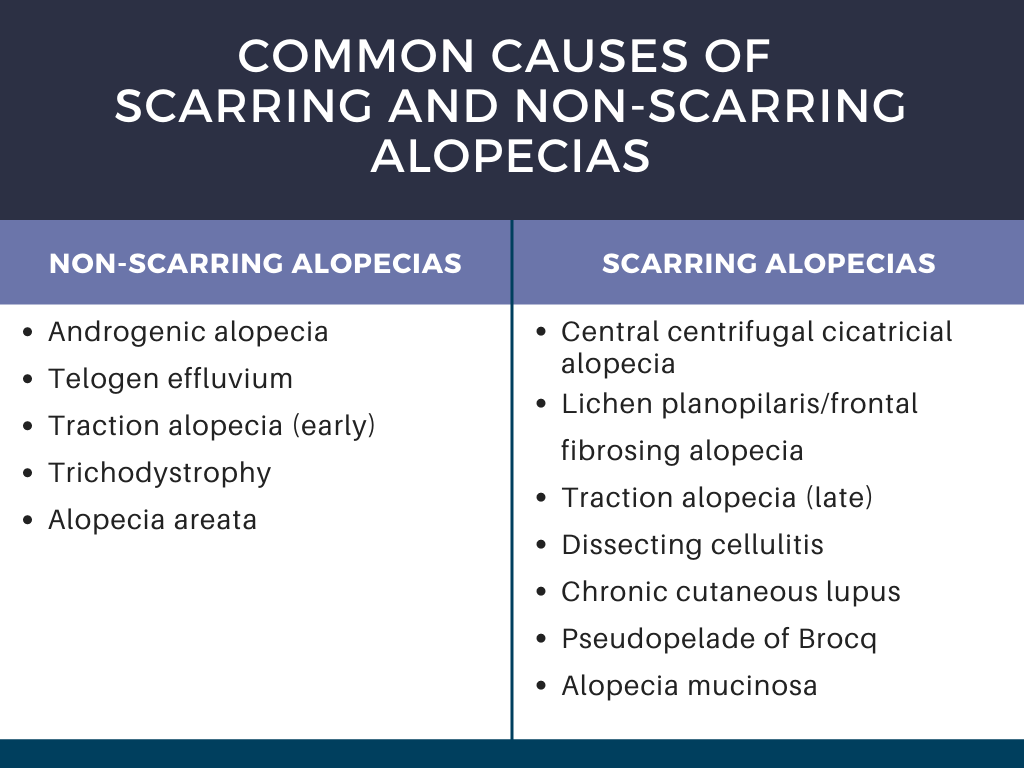
- Accurately diagnose the disease (see Table 1 for common causes of alopecia)
- Effectively and competently partner with the patient to treat the disorder with appropriate therapy
Dr. Taylor stressed the importance of culturally competent questioning during the visit. For example, asking an African American woman if she shampoos daily can reduce the patient’s confidence in the physician’s understanding of her hair type, especially during a race discordant visit. To build confidence, it is critical to understand routine hair practices and to be familiar with common products.
During the hair loss consultation, it is important to understand the problem experienced by the patient. Frequent symptoms noted by the patient that can clue in the underlying alopecia include:
-
- Hair length is not increasing.
- There is hair breakage.
- Hair is falling out at the root.
- There is decreased hair density.
- There is focal or localized hair loss.
Other considerations include the duration of hair loss, any associated symptoms, and presence of family history of hair loss. Further, it is important to ask about their hair care history. The types of hairstyles used by the patient and the hair care routine should be discussed.
The physical exam should be thorough to evaluate the scalp and hair density, a hair pull test, and examination of the eyebrows and eyelashes. The presence of weaves, braids, or wig caps may impede evaluation. If the patient has any of these hairpieces on the scalp that cannot be easily removed during the visit, the patient should return for evaluation after these are removed. History can still be discussed during the visit, however, the co-pay should be refunded, and the patient should be offered an earlier appointment for evaluation of the hair and scalp.
Now that we have discussed how to approach the consultation, let’s get into the alopecias! Dr. Taylor highlighted central centrifugal cicatricial alopecia, traction alopecia, and frontal fibrosing alopecia, as well as tips to minimize breakage, reduce hair tension, and scalp care to treat seborrheic dermatitis.
Central centrifugal cicatricial alopecia (CCCA) is a scarring alopecia seen in about 5.6% of African American women. It frequently starts with increased hair breakage at the vertex, and patients often have associated symptoms of itching, burning, tenderness, and soreness of the scalp. The goals of treatment are to aggressively treat the CCCA in the early stages to prevent progression, relieve symptoms, and possibly have some regrowth in the affected areas. There are no randomized controlled trials for CCCA treatment, thus evidence for treatment comes from case reports and series. The mainstay of treatment is corticosteroids (topical and intralesional), anti-inflammatory antibiotics, antimalarials, and minoxidil (topical and oral formulations). Anti-seborrheic shampoos, hair transplantation, and platelet-rich plasma injections serve as adjuncts to treatment. See Table 2 for detailed treatment options. Frequently multiple agents are used in combination to control the disease.
Two important areas of focus when treating CCCA that Dr. Taylor highlighted are practices to minimize hair breakage and treatment of frequently concurrent seborrheic dermatitis.
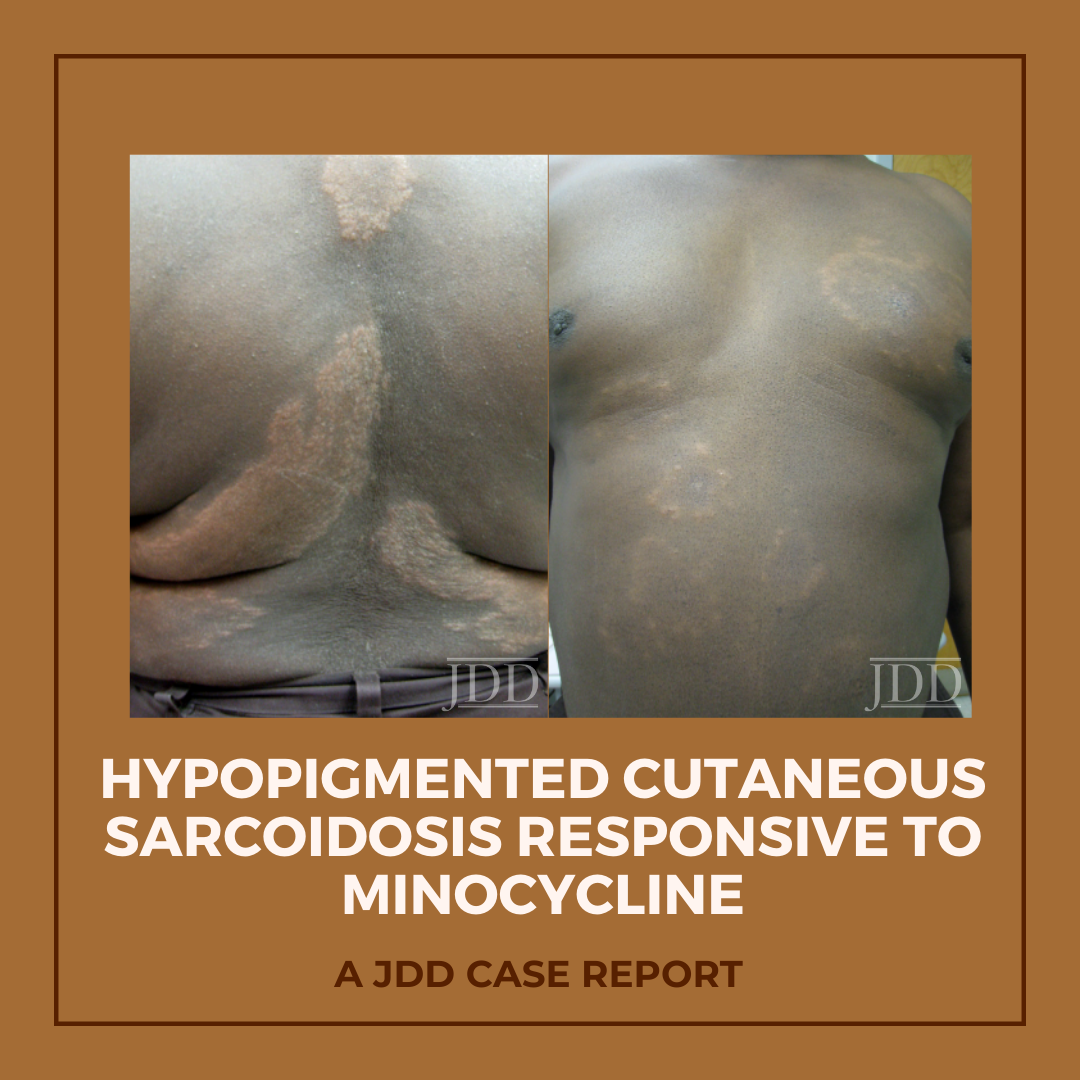
Hypopigmented patches and plaques are a rare presentation of cutaneous sarcoidosis. JDD authors describe a case of generalized hypopigmented cutaneous sarcoidosis that showed good response to minocycline therapy.
Introduction

FIGURE 1. Hypopigmented plaques over the back.

FIGURE 2. Hypopigmented annular plaques of papules on the abdomen.
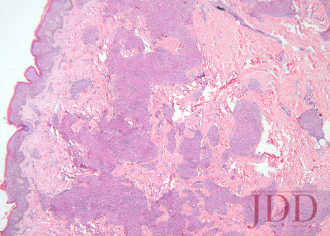
FIGURE 3. Hematoxylin and eosin stain of a left arm skin biopsy show-ing dermal granulomatous inflammation.
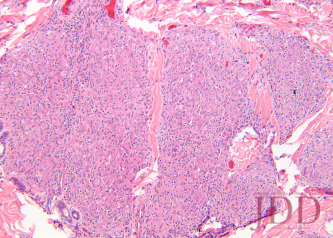
FIGURE 4. Hematoxylin and eosin stain of a left arm skin biopsy at higher magnification demonstrating well-formed naked granulomas.

FIGURE 5. Flattening and repigmentation of plaques on the back after treatment with minocycline.

FIGURE 6. Repigmentation of annuli on the anterior trunk after treat-ment with minocycline.
Discussion
The skin is one of myriad organs potentially affected by sarcoidosis, a multisystem idiopathic disorder characterized histologically by infiltration of noncaseating granulomas. Cutaneous manifestations of sarcoidosis are protean, including papules and plaques of various morphology and distribution, subcutaneous nodules, pruritus, ichthyosis, erythroderma, ulceration, verrucosis, nail disease, and infiltrative scars.1 In the United States, sarcoidosis is more common in African-Americans than in other ethnic groups, and cutaneous manifestations in individuals of African descent are more likely to be atypical.2
Minocycline as monotherapy was efficacious for the treatment of chronic cutaneous sarcoidosis in an open observational study of 12 patients by Bachelez et al.17 The cutaneous manifestations of patients in the Bachelez group included classic plaques, papulonodules, subcutaneous nodules, and lupus pernio. Ten of 12 patients completely or partially responded to treatment, which was generally well tolerated except for drug hypersensitivity syndrome in one patient with a history of other autoimmune diseases. Park et al later reported a patient with cutaneous, lacrimal gland, pulmonary, and ocular (choroidal) sarcoidosis that responded to minocycline.18
Conclusion
Disclosures
References
- English JC 3rd, Callen JP. Sarcoidosis. In: Callen JP, Jorizzo JL, Bolognia JL, et al, eds. Dermatological Signs of Internal Disease. 4th ed. China: Elsevier; 2009:287-295.
- Jayck WK. Cutaneous sarcoidosis in black South Africans.Int J Dermatol. 1999;38(11):841-845.
- Cornelius CE 3rd, Stein KM, Hanshaw WJ, Spott DA. Hypopigmentation and sarcoidosis. Arch Dermatol.1973;108(2):249-251.
- Hubler WR Jr. Hypomelanotic canopy of sarcoidosis. Cutis.1977;19(1):86-88.
- Alexis JB. Sarcoidosis presenting as cutaneous hypopigmentation with repeatedly negative skin biopsies.Int J Dermatol. 1994;33(1):44-45.
- Hall RS, Floro JF, and King LE Jr. Hypopigmented lesions in sarcoidosis. J Am Acad Dermatol. 1984;11(6):1163-1164.
- English JC 3rd, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44(5):725-743.
- Clayton R, Breathnach A, Martin B, et al. Hypopigmented sarcoidosis in the Negro. Report of eight cases with ultrastructural observations. Br J Dermatol.1977;96(2):119-125.
- Sapadin AN, Fleischmajer R. Tetracyclines: nonantibiotic properties and their clinical implications. J Am Acad Dermatol. 2006;54(2):258-265.
- Stone M, Fortin PR, Pacheco-Tena C, Inman, RD. Should tetracycline treatment be used more extensively for rheumatoid arthritis? Metaanalysis demonstrates clinical benefit with reduction in disease activity J Rheumatol.2003;30(10):2112-2122.
- Falk ES. Sarcoid-like granulomatous periocular dermatitis treated with tetracycline. Acta Derm Venereol.1985;65(3):270-272.
- Camacho F, García-Bravo B, and Carrizosa A. Treatment of Miescher’s cheilitis granulomatosa in Melkersson-Rosenthal syndrome. J Eur Acad Dermatol Venereol.2001;15(6):546-549.
- Mullanax MG, Kierland RR. Granulomatous rosacea. Arch Dermatol. 1970;101(2):206-211.
- Senet P, Bachelez H, Ollivaud L, Vignon-Pennamen D, Dubertret L. Mi- nocycline for the treatment of cutaneous silicone granulomas. Br J Dermatol. 1999;140(5):985-987.
- Marcus DV, Mahmoud BH, Hamzavi IH. Granuloma annulare treat- ed with rifampin, ofloxacin, and minocycline combination therapy Arch Dermatol. 2009;145(7):787-789.
- Duarte AF, Mota A, Pereira MA, Baudrier T, Azevedo F. Generalized granuloma annulare—response to doxycycline.J Eur Acad Derma- tol Venereol. 2009;23(1):84-85.
- Bachelez H, Senet P, Cadranel J, Kaoukhov A, Dubertret L. The use of tetracyclines for the treatment of sarcoidosis.Arch Dermatol. 2001;137(1):69-73.
- Park DJ, Woog JJ, Pulido JS, Cameron JD. Minocycline for the treatment of ocular and ocular adnexal sarcoidosis.Arch Ophthal- mol. 2007;125(5):705-709.
- Miyazaki E, Ando M, Fukami T, Nureki S, Eishi Y, Kumamoto T. Mi- nocycline for the treatment of sarcoidosis: Is the mechanism of action immunomodulating or antimicrobial effect? Clin Rheumatol. 2008;27(9):1195-1197.
- Tchernev G. Cutaneous sarcoidosis: the “great imitator”: etiopathogenesis, morphology, differential diagnosis, and clinical management. Am J Clin Dermatol. 2006;7(6):375-382.
- Marshall TG, Marshall FE. Sarcoidosis succumbs to antibiotics—implications for autoimmune disease.Autoimmun Rev.
- Webster GF, Toso SM, and Hegemann L. Inhibition of a model of in vitro granuloma formation by tetracyclines and ciprofloxacin. Involvement of protein kinase C. Arch Dermatol. 1994;130(6):748-752.
Originally published in the Journal of Drugs in Dermatology in April 2012.
Schmitt, C. E., Fabi, S. G., Kukreja, T., & Feinberg, J. S. (2012). Hypopigmented cutaneous sarcoidosis responsive to minocycline. Journal of drugs in dermatology: JDD, 11(3), 385-389. https://jddonline.com/articles/dermatology/S1545961612P0385X
Content and images republished with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
The Journal of Drugs in Dermatology is available complimentary to US dermatologists, US dermatology residents, and US dermatology NP/PA. Create an account on JDDonline.com and access over 15 years of PubMed/MEDLINE archived content.
Did you enjoy this case report? You can find more here.


