What is Rosacea?
Rosacea is a common chronic inflammatory skin disease that primarily impacts the face, and includes papules, pustules, erythema, telangiectasias, perilesional redness, phymatous changes, and even eye involvement. Symptoms may vary among different patients and even vary over time in an individual patient. Central facial redness affects many adults and can be an indicator of the chronic inflammatory disease rosacea. Rosacea is a clinical diagnosis based on the patient’s history, physical examination, and exclusion of other disorders.
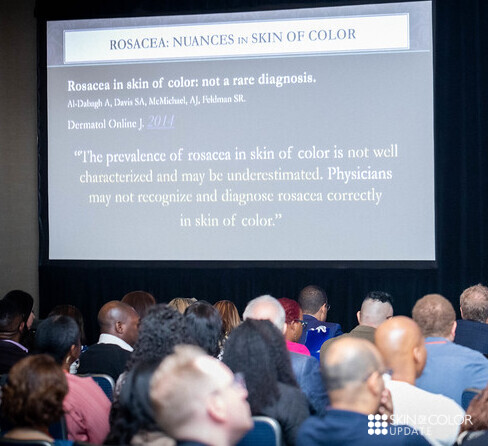
Rosacea is often under-diagnosed, particularly in individuals with skin of color. As a result, Skin of Color Update held a lecture on the topic at the most recent event.
Rosacea: Nuances in Clinical Presentation and Treatment
At Skin of Color Update 2019, Dr. Fran Cook-Bolden aimed to catch us all up to speed in how to recognize rosacea in more richly pigmented skin. Her lecture on Rosacea: Nuances in Clinical Presentation and Treatment was brimming with practical tips on how to identify the often subtle and overlooked ways that rosacea can manifest in skin of color. The following is an excerpt of an article by Kimberly Huerth, MD published on Next Steps in Derm.
Because rosacea can have a nuanced presentation in skin of color (SOC), with erythema and telangiectasias that may be difficult to discern in the setting of increased background pigmentation, it was incorrectly assumed for a long time to simply not be there. The reality is that the prevalence of rosacea in SOC is not well characterized but is likely underestimated.1Dermatologists who see a large number of SOC patients, however, will tell you that rosacea is by no means rare in this population. And I am one of these dermatologists—at my Howard University clinic, where I see predominantly black and Hispanic patients, I see several of cases of rosacea every week.
And because a diagnosis not considered is a diagnosis not made, there is often unnecessary progression of rosacea in SOC patients that results from delayed and/or inaccurate diagnosis, which in turn engenders inappropriate or inadequate treatment. As a consequence, this can lead to morbidity in the form of disfiguring, occasionally irreversible cutaneous findings, as well as intense and chronic emotional distress.
Pearls
- Look for the nuanced clinical findings!!
- Fixed centrofacial erythema may appear more reddish/violet
- A patient complains of “acne,” but has no comedones. Additionally, papules and pustules are superimposed on an erythematous background. Inflammatory papules may also appear on the chest and back.
- Telangiectasias can be difficult to appreciate with the naked eye in FST V – VI, so use your dermatoscope to help you find them
- Check for scleral injection, which may be a sign of ocular rosacea. Be aware that the onset of ocular findings may proceed cutaneous ones.
- Phymatous rosacea is a giveaway!
- Facial edema of the upper 2/3 of the face in a patient who has complained of longstanding rosacea symptoms may represent progression to Morbihan disease. Case in point (quite literally)—a poster that I presented at the Skin of Color Update highlighted a case of Morbihan disease in a black man who had reported symptoms of rosacea to his non-dermatology providers for 16 YEARS before he came to see me and received a correct diagnosis. To learn more about this case, and Morbihan disease, check out Dr. Lola Adekunle’s interview on Next Steps in Derm.
- Pertinent negatives are just as important as pertinent positives. Know that post-inflammatory hyperpigmentation (PIH) is ALMOST NEVER directly related to rosacea, unless the disease is very chronic and severe OR if the patient has been injured their skin in some way while trying to self-treat disease manifestations (picking at lesions, using harsh topical therapies)
For more rosacea pearls and AHA moments, visit the article on Next Steps in Derm.
Purchase lectures like this one: